90% of adults don’t have optimal vitamin D levels which can increase the risk of several health conditions…
Vitamin D is the sunshine vitamin because it is produced in the skin when you are exposed to the sun’s UV rays. Where you live directly increases your risk of vitamin D deficiency. For example, people who live above 40º North latitude (e.g., New York City) don’t have enough exposure to UV radiation between October and May to synthesize vitamin D.
Even during months when enough UV is available to produce vitamin D, types of clothing, shift work and time spent indoors away from the sun and heat can result in less skin exposure.
Where does vitamin D come from?
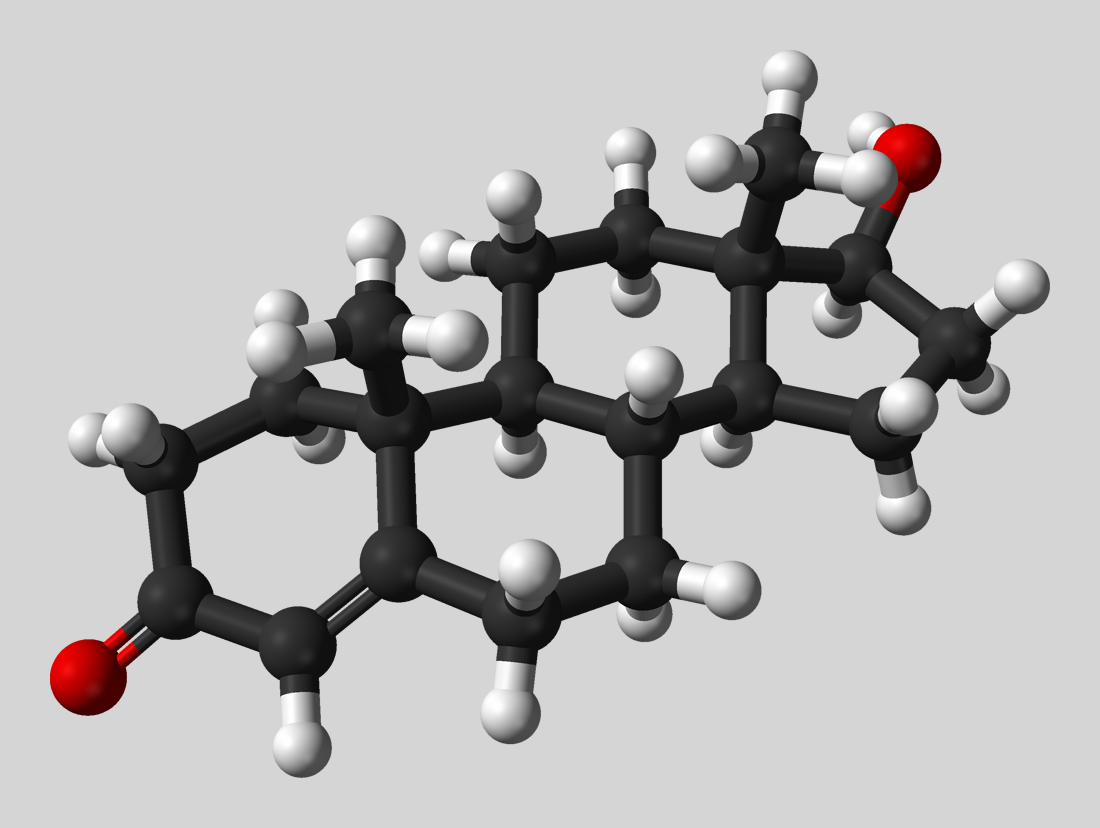
When our skin is exposed to the sun’s UV rays changes the structure of cholesterol in our skin to pre-vitamin D. Pre-vitamin D is then modified again in the skin through chemical reactions to become cholecalciferol or more commonly referred to as vitamin D3. Cholecalciferol is then released from the skin into the blood where it is then changed into active vitamin D3 by the kidneys.
Vitamin D can also be sourced from different foods in our diet. Vitamin D3 is also found in foods like eggs, yolks, fish, and cheese. During digestion, these also must go through a similar process of conversion in the body much like vitamin D produced in the skin.
Like many processes in the body, the production of vitamin D is complicated and there are many different aspects of our health that can impact vitamin D status.
How does vitamin impact my health?
One of the primary functions of vitamin D is supporting bone health. Vitamin D works to maintain calcium and phosphorus levels in the blood. When blood calcium levels drop too low, vitamin D tells your digestive system to absorb more calcium and tells the kidneys to hold on to calcium and not release it into the urine.
Not surprisingly then, low vitamin D levels are associated with osteoporosis.
Vitamin D deficiency also affects a wide range of other health conditions including increasing the risk of colon, breast, ovarian, and prostate cancer, worse pregnancy outcomes, higher blood pressure, immune system issues, diabetes, cardiovascular disease, obesity, and depression.
European Caucasians demonstrate lower rates of deficiency compared with non-white individuals who require more sun exposure to produce equivalent cholecalciferol from the skin. Even countries with populations who have access to greater sun exposure report a high prevalence of vitamin D deficiency; more than 20% of the population are deficient in India, Tunisia, Pakistan, and Afghanistan. Occupational factors such as shift work can also play a role along with ethnicity in different regions.
Your optimum health takeaway
References:
Anglin, R. E., Samaan, Z., Walter, S. D., & McDonald, S. D. (2013). Vitamin D deficiency and depression in adults: systematic review and meta-analysis. British Journal of Psychiatry, 202, 100-107.
Amrein, K., Scherkl, M., Hoffmann, M., Neuwersch-Sommeregger, S., Kostenberger, M., Tmava Berisha, A., Malle, O. (2020). Vitamin D deficiency 2.0: an update on the current status worldwide. European Journal of Clinical Nutrition, 74(11), 1498-1513.
Earthman, C. P., Beckman, L. M., Masodkar, K., & Sibley, S. D. (2012). The link between obesity and low circulating 25-hydroxyvitamin D concentrations: considerations and implications. International Journal of Obesity (London), 36(3), 387-396.
Keum, N., & Giovannucci, E. (2014). Vitamin D supplements and cancer incidence and mortality: a meta-analysis. British Journal of Cancer, 111(5), 976-980.
Spedding, S. (2014). Vitamin D and depression: a systematic review and meta-analysis comparing studies with and without biological flaws. Nutrients, 6(4), 1501-1518.