Our daily lives expose us to many things that can decrease our testosterone levels... Here are the top 6 silent killers of testosterone that you need to be aware of and the essential strategies to manage them.
1. Body fat
Excess body fat is most commonly linked to diabetes and cardiovascular disease, BUT body fat also decreases testosterone. start
Elevated levels of body fat start a process where testosterone is converted into estrogen. Increased levels of estrogen promote greater fat deposits in our bodies creating a ‘downward spiral’ of continually lowering testosterone and increasing fat.
Increased levels of body fat also decrease the amount of sex hormone-binding globulin (SHBG), a hormone that is responsible for carrying testosterone to our cells. This results in a greater clearance of testosterone from our bodies rather than going to the intended target cells.
2. Sugary foods
Throughout the day, testosterone levels fluctuate, something known as diurnal variation. This includes a natural post-meal decrease of testosterone that occurs after eating. On average, the amount of testosterone in the blood decreases approximately 18-25% one hour after a meal and climbs back up to normal values afterwards.
Research has shown that this natural post-meal decrease is exaggerated after eating considerable amounts of sugar. Though a greater temporary decrease in testosterone won’t necessarily kill testosterone levels, if there is a consistently lower decrease due to a regular high intake of sugar, this could result in an overall lower amount of circulating testosterone over time.
Compound that with the fact that eating sugar regularly can increase your body fat levels and impact your insulin sensitivity – two things that are closely related to testosterone levels – it’s best practice to avoid high sugar intake.
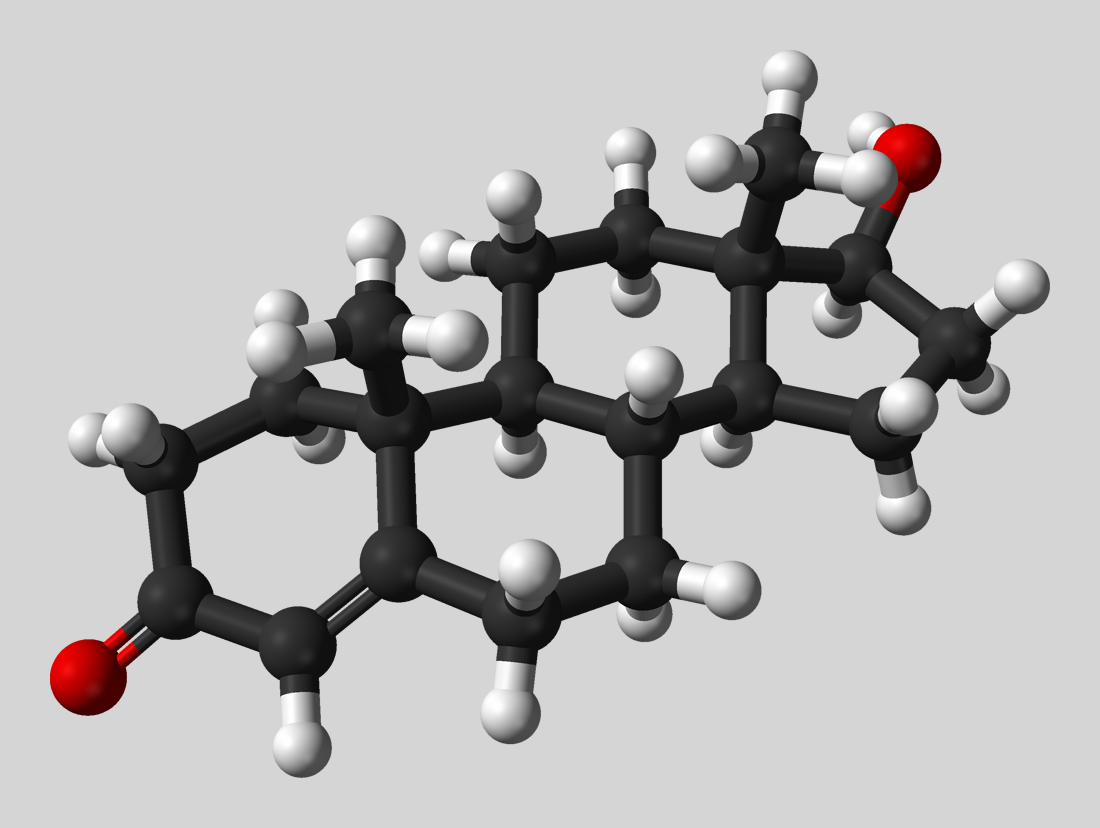
3. Endocrine disruptors
Xenoestrogens are substances that imitate estrogens and are found in both synthetic compounds like bisphenol A (BPA), polychlorinated biphenyls (PCB), and phthalates in addition to natural chemical compounds that come from plants (phytoestrogens). They can interact with estrogen receptors in the body.
Also known as endocrine disruptors, chemicals such as BPAs, PCBs, and phthalates are synthetic xenoestrogens that have been shown to damage Leydig cells, which are the testicular cells responsible for testosterone production. Additionally, these compounds can promote cancer, particularly in prostate cells.
These compounds have been commonly used to make plastics (BPA’s), plastic coatings (phthalates), or pesticides (PCBs) and can be found in lotions, pastes, and scented products. A 2017 scientific review on endocrine disruptors recommended avoiding some lotions, perfumes/colognes as well as using prepackaged foods and plastics that could leach these compounds onto products we apply on our skin or ingest. Additionally, they recommend avoiding too much of a sole source of these substances by eating a balanced diet. This advice is particularly important for women who are trying to get pregnant or are pregnant, as this type of exposure can affect fetal development.
Though none of these practices are guaranteed to eliminate endocrine disruptors from our life, they may mitigate the intake and prevent diminished testosterone levels as a result.
4. Prescription Medications
Some of the medications that we use daily can decrease our testosterone levels. Over-the-counter non-steroidal anti-inflammatory medication like ibuprofen (NSAIDs) has been shown to lower testosterone, particularly in obese and inactive men. NSAIDs can suppress the cells in testicles that are necessary for testosterone and sperm production.
Other medications such as statins can also lower testosterone, though it’s important to consider that the drugs are given to treat cardiovascular disease, so the benefits of use supersede the diminished testosterone levels.
5. Alcohol
Alcohol intake has varied effects on acute levels of testosterone in men. Heavy drinking (which can be defined as 15 or more drinks per week for men) decreases blood testosterone, and studies have shown that even sitting, consuming 2.5ml/kg of bodyweight of vodka in 15 minutes suppressed testosterone levels. Though some studies demonstrate lesser amounts of alcohol may cause a temporary increase, long-term alcohol intake has negative effects on the Leydig cells, which are the cells in the testicles that produce testosterone.
In general, occasional low to moderate intake of alcohol (defined as 0-2 drinks) won’t have any detrimental effects on testosterone compared with heavier regular drinking.
6. Stress
The daily pressures of life combined with a lack of sleep can have serious effects on testosterone production. Elevated levels of stress increase the production of a hormone called cortisol, a hormone secreted by the adrenal glands in response to physical and psychological stress. This is a normal response to stress as cortisol helps keep our body fueled by stimulating the production of glucose.
However, chronically elevated levels of cortisol can have detrimental effects on testosterone production. Cortisol has been demonstrated to directly lower testosterone.
Using stress management tools and getting enough sleep can counteract these chronic effects.
Paradoxically, though exercise increases cortisol, it’s one of the few stressors where there doesn’t seem to be the same type of relationship between cortisol and testosterone, making it another valuable tool to manage stress and prevent a decline in testosterone.
References:
- Braun JM. Early-life exposure to EDCs: role in childhood obesity and neurodevelopment. Nat Rev Endocrinol. 2017;13(3):161-73.2.
- Brownlee KK, Moore AW, Hackney AC. Relationship between circulating cortisol and testosterone: influence of physical exercise. J Sports Sci Med. 2005;4(1):76-83.
- Caronia LM, Dwyer AA, Hayden D, Amati F, Pitteloud N, Hayes FJ. Abrupt decrease in serum testosterone levels after an oral glucose load in men: implications for screening for hypogonadism. Clin Endocrinol (Oxf). 2013;78(2):291-6.
- Gao H, Yang BJ, Li N, Feng LM, Shi XY, Zhao WH, et al. Bisphenol A and hormone-associated cancers: current progress and perspectives. Medicine (Baltimore). 2015;94(1):e211.
- Gates MA, Araujo AB, Hall SA, Wittert GA, McKinlay JB. Non steroidal anti-inflammatory drug use and levels of oestrogens and androgens in men. Clin Endocrinol (Oxf). 2012;76(2):272-80.
- Goncalves GD, Semprebon SC, Biazi BI, Mantovani MS, Fernandes GSA. Bisphenol A reduces testosterone production in TM3 Leydig cells independently of its effects on cell death and mitochondrial membrane potential. Reprod Toxicol. 2018;76:26-34.
- Goncharov A, Rej R, Negoita S, Schymura M, Santiago-Rivera A, Morse G, et al. Lower serum testosterone associated with elevated polychlorinated biphenyl concentrations in Native American men. Environ Health Perspect. 2009;117(9):1454-60.
- Kristensen DM, Desdoits-Lethimonier C, Mackey AL, Dalgaard MD, De Masi F, Munkbol CH, et al. Ibuprofen alters human testicular physiology to produce a state of compensated hypogonadism. Proc Natl Acad Sci U S A. 2018;115(4):E715-E24.
- Nakamura D, Yanagiba Y, Duan Z, Ito Y, Okamura A, Asaeda N, et al. Bisphenol A may cause testosterone reduction by adversely affecting both testis and pituitary systems similar to estradiol. Toxicol Lett. 2010;194(1-2):16-25.
- Sarkola T, Eriksson CJ. Testosterone increases in men after a low dose of alcohol. Alcohol Clin Exp Res. 2003;27(4):682-5.
- Sniderman AD, Thanassoulis G. Do statins lower testosterone and does it matter? BMC Med. 2013;11:58.
- Schwartz A, Patel BP, Vien S, McCrindle BW, Anderson GH, Hamilton J. Acute decrease in serum testosterone after a mixed glucose and protein beverage in obese peripubertal boys. Clin Endocrinol (Oxf). 2015;83(3):332-8.